It has many causes, and people respond to it in many ways. We have listed the most common types of pain which patients experience while being on dialysis treatment.
Pain

Pain is a complex symptom and common amongst dialysis patients. Pain is one way the body tells you something's wrong and needs attention. But pain – whether it comes from a broken bone or a long-term illness – is also something that feels bad both physically and emotionally.
Chronic pain
When pain last over a longer period – even month or years – it is commonly referred to as Chronic Pain. It interferes with daily life and can lead to a severe physical, social or psychological impact. There are multiple medical causes for chronic pain, which dialysis patient may experience. Chronic pain can for instance be caused by complications related to diabetes, arthritis, and carpel tunnel syndrome.
If pain remains unmanaged, it can cause depression or anxiety. Therefore, as first step, identifying the individual cause of pain is crucial. Pain is rarely treated with one type of therapy alone. The different therapy types may include medications, injection therapies, massage, physical therapy, icing sprays, relaxation techniques or acupuncture.
Particularly for the intake of medications or injections, it is crucial to ensure safety in your therapy as dialysis patient. Together with your medical team, the right approach to pain management can be found. Please do not take any medications which are not aligned with your treating physician.
The most successful treatment for pain comes from using multiple methods of pain management. Pain specialists can help you develop these comprehensive plans.
Deep Breathing Exercise

Before You Begin
Find a quiet space where you won’t be interrupted. Lie down or sit comfortably; try to relax your body as much as possible. Close your eyes. Scan your body for tension.
Start out by simply bringing your attention to your breathing. Place one hand on your abdomen, and one hand on your chest. Notice which hand is moving, and how fast it is moving. If you are anxious, your breath trends to be quicker and shallow.
Getting Started
Begin by taking a slow, easy, mindful breath in, through your nose, gently pulling the air deep down into your abdomen. You should feel your abdomen rise with this inhalation and your chest should only move a little.
- Inhale for a count of 5. Hold that breath deep in your lungs for a count of two. Slowly exhale, making sure to keep your mouth relaxed.
- Exhale for a count of 5-7. It is important to remember that we deepen our breath by completely emptying our lungs on an exhale, not by filling them with more air on an inhale.
Imagine
When you inhale, picture you fill your lungs in 3 stages:
Air entering your nose and travelling past your throat
Focus on the air filling up your chest
Your abdomen and belly raise as your breath fills your lungs
As you exhale, focus on the same three stages in reverse order. Ideally practice deep breathing twice per day, for 7-10 minutes. Set an alarm so you don’t need to worry on the time.
Please note
Sometimes, you may start to feel lightheaded. This sensation simply means that your brain is getting more oxygen than it needs. If this happens to you, simply take a break from the exercise, and breathe normally. This exercise does not replace a consultation of your care team or other therapy options!
Reduction of blood circulation in your hand
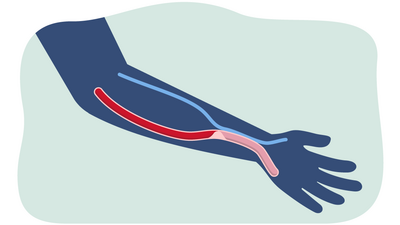
Steal syndrome is a rare complication that can occur after the construction of a vascular access. It is caused by a lack of blood supply and circulation in the hand due to the creation of a fistula.
When constructing a vascular access, the arterial blood that would normally flow to your hand also flows through the fistula. Thus, the blood is shared between your hand and the fistula. This can result in less blood flowing into your hand. The decreased blood flow can result in your hand becoming cold, numb, blue, weak, and painful. Symptoms often worsen during dialysis or in cold weather.
In very severe cases, an extreme lack of blood can lead to tissue damage and non-healing ulcers and gangrene over time. This situation poses a high risk of infection, which can spread throughout the body via the blood. To prevent this, surgical intervention might be needed. Depending on the severity of the syndrome, different treatment methods need to be applied.
Treating steal syndrome

Steal syndrome is diagnosed based on your communication, physical examination and imaging methods. Depending on the severity of the syndrome, conservative treatment or a surgical intervention is applied. Commonly patients only suffer from mild symptoms such as cold hands. In this case, steal syndrome does not require specific interventions, but only close observation of the symptoms to early detect any deteriorations.
Gloves and hand exercise can help alleviate symptoms.
In cases of severe steal syndrome, a surgical intervention may be necessary. Through a surgical intervention adequate blood flow in the hand can be restored. This can result in relieve of symptoms and prevention of irreversible tissue damage.
How can you help yourself?


You can play a part in your care and help manage cold or numb hands:
Use gloves when your hands are cold. This is an easy way to warm your hands and to reduce pain due to cold hands.
Make small movements or exercises with your hand when it is cold or numb. Thus, you can activate blood circulation in your hand. You can do this both during dialysis and at home.
- Work together with your care team. Everyone's body and health are different. It is essential that you follow the individualised instructions given by your care team. They will determine which specific needs you have and support you in controlling your condition. Inform your dialysis care team if you have any symptoms on your hand on the side of the vascular access. Your care team will evaluate treatment options and select the most suitable care for you.
Hemodialysis muscle cramps

Common but usually harmless complication of dialysis treatment
Muscle cramp is the sudden, unintentional and often painful tensioning of the muscle. Muscle cramps occur when muscles uncontrollably and unintentionally contract or tighten.
Muscle cramps are a common complication of dialysis treatment. They frequently occur at the end of a dialysis treatment. All muscles can be affected by muscle cramps, but most commonly muscle cramps take place in the legs.
During dialysis, muscle cramps are caused mainly by fluid loss and change in electrolyte balance. Taking out a lot of fluid results in low blood volume and a change of the balance of electrolytes such as sodium, potassium, magnesium and calcium. This may cause muscle cramps. Muscle cramps usually only last a few seconds. They can cause sudden and severe pain, but they are generally not harmful.
Managing risks & finding treatment solutions
Muscle cramps can lead to sudden and severe pain. In some cases, they can be so painful that the dialysis session needs to be stopped. You should alert staff as soon as the cramp begins, so that appropriate interventions can be implemented before the cramp becomes severely painful. Your care team may prescribe medication or adjust your current treatment session to ease the pain of muscle cramps. The best treatment is prevention of muscle cramps through personalized treatment prescription. Your care team will evaluate the treatment possibilities and apply the best-suitable care.
What can you do in your daily life to prevent muscle cramps?
-
Daily stretching
-
Low intensity exercise
-
Follow your recommended diet & fluid intake between dialysis treatments
-
What can you do to ease the pain of muscle cramps during dialysis?
-
Massage or stretch the cramped muscle
-
Light exercise
-
Be aware of the signs of cramps and alert staff early
Stretching improves overall health

Stretching is safe for most people with chronic kidney disease, and it is good for your health.
It is important to stretch the major muscle groups. Stretching can help reduce muscle cramps. Moreover, it enhances your overall physical fitness. Stretching improves the movement of joints, reduces stiffness in muscles and helps you reduce stress.
Stretching rules
Start slowly and progress gradually
It is important to keep breathing during stretching
Stretching should be done
15-20 min and 4-7 times a weekStop the exercise immediately if you feel one of the following symptoms: shortness of breath, irregular racing heartbeat, nausea, dizziness, lightheadedness, excessive fatigue, blurred vision
Always talk to your dialysis care team about starting exercise

